I have been asked to talk about the role of Vitamin K (K2 specifically) in the pathogenesis of vascular disease. This is a controversial topic as “mainline cardiology” has not yet embraced the data and the “jury” is not yet out as to the importance of vitamin K2 in preventing and treating cardiovascular disease. The data I will summarise is extremely interesting and I believe we will be incorporating this knowledge into prevention and management of atherosclerotic vascular disease soon.
Introduction:
We have been conventionally taught that the role of vitamin K was solely ascribed to coagulation and coagulation was thought to be involved only in the venous system.
This view has dramatically changed with the recent (last decade) discovery of vitamin K-dependent proteins outside the coagulation cascade and the role of coagulation factors in the pathogenesis of atherosclerosis on the arterial side. Vitamin K-dependent proteins are involved in the regulation of vascular smooth muscle cell migration, apoptosis (programmed cell death), and vascular calcification.
Vascular calcification is a well recognised important independent predictor of cardiovascular disease and closely correlates cardiac morbidity and mortality. The involvement of vitamin K-dependent proteins such as matrix Gla-protein (MGP) in vascular calcification makes that calcification amendable for intervention with high intake of vitamin K2.
Nutritional vitamin K consists of two forms:
-
vitamin K1 (a phylloquinone also known as phytonadione)
- vitamin K2 (a menaquinone)
Vitamin K1 is found in leafy green vegetables (lettuce, spinach and broccoli)where it is tightly bound to the chloroplast membrane resulting in a poor absorption (poor bio-availability) of vitamin K1 from vegetables but it is still the dominant form making up about 90% of the vitamin K in a typical Western diet.
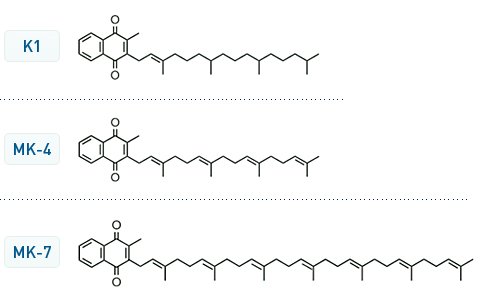
Vitamin K2 is found in fermented foods such as cheese, sauerkraut and the Japanese Natto (a foul-smelling sticky web of fermented soybeans typically served with a Japanese breakfast.derived from the bacterium Bacillus subtilis). The absorption of vitamin K2 is apparently much better as compared to vitamin K1 comprising 10% of our vitamin K consumption. Vitamin K2 importantly can be synthesised in the colon by microflora. There are apparently 4 isoforms of vitamin K2 determined by the number of prenyl side chains (MK-4; MK-7; MK-8 & MK-9). MK-4 is found in meat whereas the MK-7 to 9 tend to come from the fermented foods.
Importantly the bioavailability of the isoforms differ with MK-4 demonstrating very poor bioavailability at a nutritional level dose compared to excellent bioavailability with MK-7.
After being absorbed in the intestine, vitamin K, as a fat soluble vitamin is transported by lipoproteins, as it has no specific carrier protein. The different lipophilicity (fat solubility) of K1 and K2 may result in substantial differences in plasma transport, half-life and delivery to target tissues (t1/2 for K1 ~ 3 hours; 1.5 hours for MK-4 and > 70 hours for MK-7; MK-8 & MK-9).
Vitamin K-dependent proteins:
Vitamin K-dependent proteins constitute a family of 16 known proteins with diverse functions, not only involved in the haemostatic coagulation pathway. The vitamin K dependent coagulation proteins (clotting factors II, VII, IX and X) are essential for the coagulation cascade and are γ-carboxylated in the liver to be functionally active. They are well-balanced by the anticoagulant factors protein C and protein S.
All these vitamin K-dependent proteins are mainly synthesized and γ-glutamylcarboxylated in the liver, with the exception of proteins S which is synthesized in part by endothelial cells.
Over the past decade an enormous amount of evidence has suggested that coagulation factors play an important role in (chronic) inflammation. Phagocytosis of apoptotic cells by macrophages is thought to limit the inflammatory response and Protein S has been identified as a factor responsible for stimulation of this phagocytosis. Additionally protein S regulates the expression and function of scavenger receptor A (SR-A) on macrophages resulting in diminished uptake of acetylated low density lipoprotein.
Protein C deficiency is associated with severe coagulation response to endotoxin and this Protein C also plays a significant role in the inflammatory response with activate Protein C inhibiting endotoxin-induced production of important cytokines like TNF-alpha, IL-1, IL-6 and Il-8 by momocytes/macrophages.
Extrahepatic vitamin K-dependent proteins:
Within the arterial vessel wall vitamin K-dependent proteins are synthesized with functions not related to blood coagulation.
Growth arrest specific gene 6 protein (Gas-6) is a vitamin K-dependent protein produced by vascular smooth muscle cells (VSMCs). Gas-6 seems to protects VSMCs from calcification by inhibiting apoptosis as the cell death may act as a nidus for calcification.
The vitamin K-dependent matrix Gla-protein (MGP) is regarded as the strongest inhibitor of vascular calcification (VC) and produced by many cells, including VSMCs. Rescue experiments in MGP null mice demonstrated that MGP acts locally in the vascular tissue as restoration of MGP expression in arteries completely rescued the arterial mineralization phenotype, whereas hepatic MGP expression, resulting in high systemic MGP levels, did not.
Vascular calcification as a marker of atherosclerosis risk stratifies into high risk outcome:
Vascular calcification (VC) is associated with increased cardiovascular mortality and morbidity, and is recognised as a strong and independent risk factor for cardiovascular death. The amount of VC, as measured and quantified by multidetector computed tomography (CT-coronary angiography) is an important predictor of:
-
all-cause mortality
- vascular complications
- myocardial infarction and stroke
Patients with higher coronary artery calcification scores have approximately ten times more chance to have a cardiac event in the next 3–5 years. Patients with a calcification-progression over 15% per year had a 17.2 fold increased risk of myocardial infarction compared to patients without significant progression.
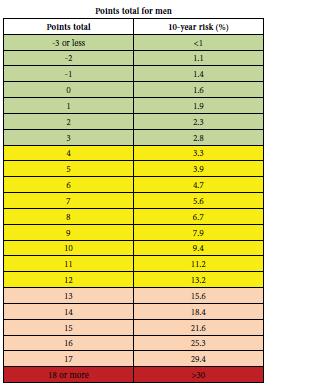
Vascular calcification is an even stronger predictor than the Framingham Risk Score (FRS) which is currently used to score 10-year risk prediction for cardiovascular events.
Clinically,VC causes stiffening of the vascular arteries via elastic fiber and VSMC calcification resulting in:
-
decreased arterial compliance with the development of chronic systemic hypertension
- development of left ventricular hypertrophy leading to diastolic heart failure
- decreased coronary perfusion
In spite of this data, calcification of arteries has been generally neglected and considered to be clinically unmodifiable, often regarded as an end stage passive process not amenable to therapeutic intervention. Recent data however suggests that punctated and spotty calcification in the atherosclerotic plaque influence stability negatively and render the plaque vulnerable to rupture thus potentiating the progression of atherosclerosis and vascular events.
As VC is a complex and actively regulated process involving cells and vitamin K dependent proteins acting as catalysts and inhibitors. Recruitment of macrophages in the atherosclerotic plaque and consequently their secretion of inflammatory cytokines may serve as a signal for intimal calcification. When VSMCs phagocytose calcium crystals it seemingly destabilize atherosclerotic plaques by initiating inflammation and by causing SMC death. 
Circulating biomarkers (MGP) for detecting vascular calcification:
This is an attractive concept to screen for and perhaps regulate mechanisms of VC. Vitamin K-dependent proteins have been associated with the earliest calcification areas in the plaque. Uncarboxylated MGP seemingly strongly correlates with both medial and intimal calcification. By measuring circulating MGP isoforms it has been shown that the majority of the healthy population have sub-optimal levels of vascular vitamin K. Preliminary data suggest that some MGP conformations are associated with aspects of cardiovascular disease for instance patients with high VC scores display high levels of inactive MGP, especially dialysis patients.
This creates possibilities for targeting VC with vitamin K therapy. Indeed high intake of vitamin K has been shown to regress preformed medial calcification in a rat model and the first data is available in dialysis patients showing that vitamin K supplementation markedly reduced the level of plasma uncarboxylated prothrombin, uncarboxylated osteocalcin and inactive MGP.
Conclusion:
Effort must be directed towards retarding or reversing the development of calcification in the vasculature, especially in those patients prone to vascular calcification (chronic kidney disease, diabetes, atherosclerotic cardiovascular disease). In these patients the treatment with vitamin K antagonists should be reconsidered perhaps with a view to used specific Thrombin inhibitors in cases where anticoagulation is required.
Therefore, it is of importance to identify patients with vascular disease and to evaluate different strategies that are more effective in the prevention of hypercoagulability as well as vascular calcification.
Here lies the real interest in high dose vitamin K2 replacement to minimise and reverse vascular calcification as part of general prevention and management of atherosclerotic vascular disease.
This is consistent with separate research also showing superior health benefits from vitamin K2, including:
- The Rotterdam Study the first study demonstrating the beneficial effect of vitamin K2, showed that people who consume 45 μg/d of K2 daily live seven years longer than people getting 12 μg/d
- Data from the Prospect EPIC Cohort published in
Nutrition, Metabolism & Cardiovascular Diseases
Gast et.al. Volume 18, Issue 7 Pages 504-510, September 2009
suggested a high menaquinone intake reduces the incidence of coronary heart disease (CHD). 16,057 women, enrolled between 1993 and 1997 and aged 49–70 years, who were free of cardiovascular diseases at baseline. Intake of vitamin K and other nutrients was estimated with a food frequency questionnaire. After a mean follow-up of 8.1±1.6 years, with 480 incident cases of CHD. Mean vitamin K1 intake was 211.7±100.3 μg/d and vitamin K2 intake was 29.1±12.8 μg/d.After adjustment for traditional risk factors and dietary factors, the authors observed an inverse association between vitamin K2 and risk of CHD with a Hazard Ratio (HR) of 0.91 [95% CI 0.85–1.00] per 10 μg/d vitamin K2 intake. This association was mainly due to vitamin K2 subtypes MK-7, MK-8 and MK-9. Vitamin K1 intake was not significantly related to CHD
Um food for thought….
Blessings Cardiologydoc